Cervical Cancer
The Cervical Working Group (CWG) consists of five modeling groups and a coordinating center. New technologies, including screening tests and vaccines against human papillomavirus (HPV), a sexually transmitted virus known to cause cervical cancer, are dramatically changing the landscape of cervical cancer control in the US and worldwide. In order to address important evidence gaps, the CWG will continue their comparative modeling collaboration to evaluate the harms, benefits, and cost-effectiveness of screening and vaccination strategies, and will disseminate findings to inform health policies and decisions.
Highlights
We adapted an existing model of cervical carcinogenesis to reflect differences in hysterectomy rates, cervical cancer screening usage, and cancer survival.
The adapted model was able to replicate observed racial disparities in cervical cancer incidence and mortality without altering assumptions on disease natural history.
HPV-based screening provides greater resilience to pandemic-related disruptions compared with cytology-based screening. Temporary delays due to the pandemic have a lesser impact on cervical cancer risk compared to the screening frequency and test modality, emphasizing the importance of consistent screening practices.
In order for regions with high prevalence to reach cervical cancer elimination goals, cervical cancer prevention and treatment strategies must be tailored to women living with HIV. Our modelling for KwaZulu Natal, South Africa, showed that screening women living with HIV every five years with Automated Visual Evaluation (AVE) or HPV DNA testing, combined with using a single-visit treatment strategy, could make it possible to reach elimination targets with the greatest reductions in cervical cancer cases compared to other strategies.
Investigators
Comparative Modeling to Inform Cervical Cancer Control Policies
Grant Number: U01CA253912
Abstract & Aims
Abstract: Despite the availability of cervical cancer screening in the United States, over 13,000 women develop and 4,000 women die from cervical cancer each year. New technologies, including screening tests and vaccines against human papillomavirus (HPV), a sexually-transmitted virus known to cause cervical cancer, are dramatically changing the landscape of cervical cancer control in the US and worldwide. As part of the Cancer Intervention and Surveillance Modeling Network (CISNET), our group of established cervical cancer modelers from the US, the Netherlands, and Australia will continue to engage in a formal collaboration of comparative modeling using state-of-the-art mathematical models of HPV and cervical carcinogenesis. We will pursue evaluations of current and forthcoming HPV vaccination and screening strategies to optimize cervical cancer control in US women, taking into account high-risk groups, existing disparities, and recent global efforts towards cervical cancer elimination, and will prioritize the dissemination of results to a broad audience of decision-makers and stakeholders.
The specific aims are to:
- To quantify the health benefits, harms, and costs of current cervical cancer prevention strategies, including HPV vaccination and screening.
- To evaluate the effectiveness and cost-effectiveness of forthcoming technologies and approaches for cervical cancer control.
- To identify efficient strategies for cervical cancer elimination among women living with HIV.
- To examine the effectiveness, efficiency, and equity of HPV vaccination and screening strategies in reducing cervical cancer disparities.
- To evaluate the potential for and timing of cervical cancer elimination as a public health problem in the US.
- To ensure wide dissemination of findings and improve transparency, understanding, and confidence in model-based analyses of cervical cancer control.
Major Analyses & Contributions
Comparative Analyses
Estimating the Natural History of Cervical Carcinogenesis
The natural history of human papillomavirus (HPV)-induced cervical cancer (CC) is not directly observable, yet the age of HPV acquisition and duration of preclinical disease (dwell time) impacts the effectiveness of prevention policies (Figure 1). We performed a comparative modeling analysis utilizing the CISNET Cervical models to characterize the age of acquisition of cancer-causing HPV infections and implied dwell times for distinct phases of cervical carcinogenesis.
In the absence of screening or vaccination, the CISNET Cervical team found the median time from HPV acquisition to cancer detection ranged from 17.5-26.0 years across the four models. Three models projected that 50% of unscreened women acquired their causal HPV infection between ages 19-23 years, while one model projected these infections occurred later (age 34 years) (Figure 2). In the context of imperfect compliance with U.S. screening guidelines, the median dwell times were shorter (12-18 years) and the median age of causal infection was 4.4-15.9 years later compared with model projections in the absence of screening. These validated CISNET-cervical cancer models, which reflect uncertainty in the development of cervical cancer, elucidate important drivers of HPV vaccination and cervical cancer screening policies and emphasize the value of comparative modeling when evaluating public health policies (Burger et al., 2019).
Figure 1: General schematic of the natural history pathway of cervical cancer for distinct preclinical dwell times
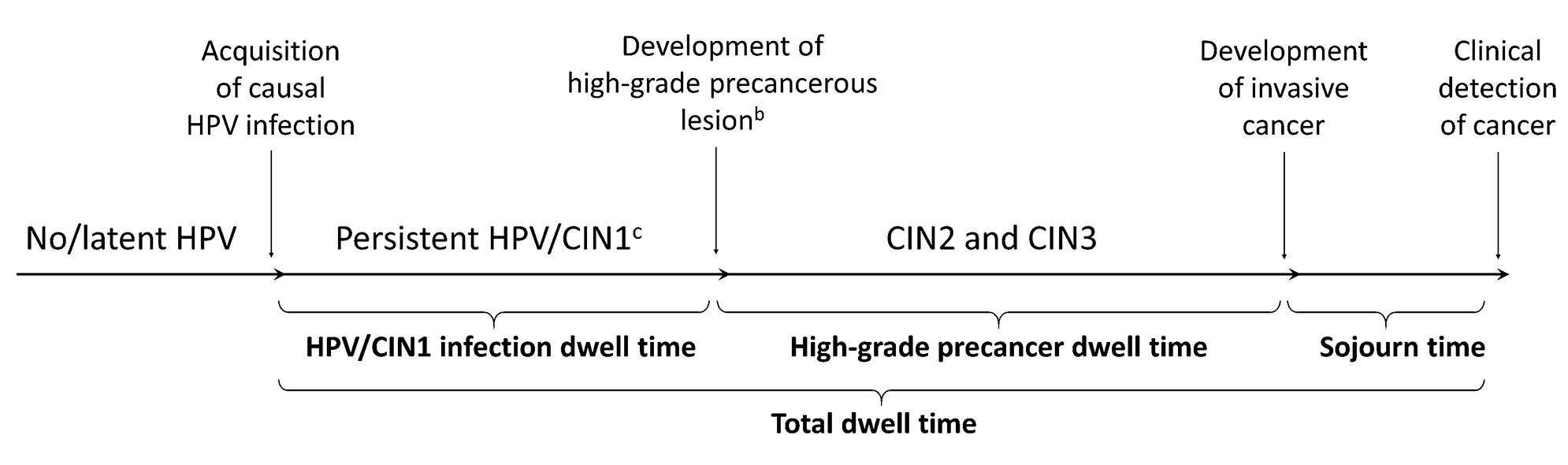
For models that allow regression from a high-grade precancer to human papillomavirus (HPV) infection and progression back to high-grade precancer prior to progressing to invasive cancer, we assumed the time spent in each health state, regardless of sequential progression contributed to the respective dwell times. Dwell time was set to zero if a woman cleared her type-specific HPV infection and any associated lesions. a The analysis stratified HPV-16, HPV-18, and other non-HPV-16/18 types; b lncludes cervical intraepithelial neoplas (CIN) grades 2 and 3; the Harvard model allow for non-sequential progression from HPV to CIN2 or CIN3; c The Harvard model does not include an explicit CIN1 health state.
Figure 1 from Burger et al., 2019, reproduced by permission of Oxford University Press (https://corp.oup.com).
Figure 2: Cumulative age of human papillomavirus (HPV) acquisition by HPV genotype for four CISNET modeling groups
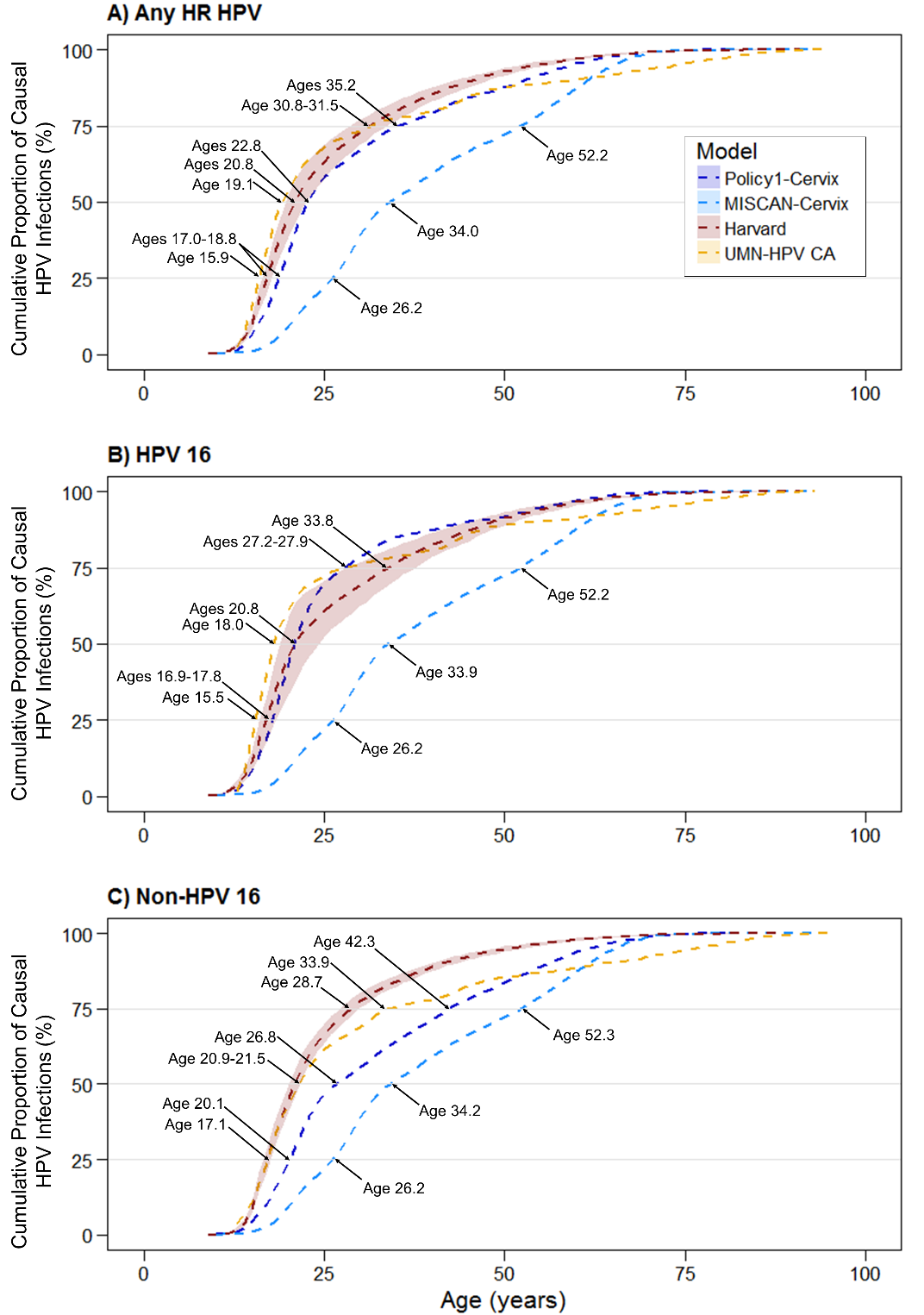
Figure 2 from Burger et al., 2019, reproduced by permission of Oxford University Press (http://global.oup.com).
Cervical Cancer Elimination in the United States
In May 2018, the World Health Organization (WHO) Director-General issued a global call to eliminate cervical cancer as a public health problem, which involves setting ambitious screening and vaccination coverage targets. The CISNET Cervical team performed a comparative modeling analysis using two of the CISNET Cervical models to assess the potential for, and timing of, cervical cancer elimination in the United States and whether this could be expedited by adopting ambitious intervention coverage targets.
We evaluated nine alternative prophylactic HPV vaccination and cervical screening scale-up scenarios compared with a ‘status quo’ scenario that involved no additional interventions. The cervical cancer elimination threshold target was defined as 4 or fewer new cases of cervical cancer per 100,000 women-years.
Under status quo assumptions, the models projected that cervical cancer incidence would fall below 4 per 100,000 women-years between 2038 and 2046 (Figure 3). Scaling up screening coverage to 90% was the most impactful intervention in terms of expediting elimination timing (10-13 years earlier), averting an average of 1,400-2,088 additional cases per year over 2019-2100. Increasing HPV vaccination coverage to 90% or vaccinating adults aged 26-45 years had minimal impacts on cervical cancer incidence.
The USA is on track to eliminate cervical cancer as a public health problem in the next two to three decades. Time to elimination could be expedited by 10–13 years by achieving higher screening coverage. [Burger et al., 2020]
Figure 3: Age-standardized cervical cancer incidence per 100,000 women-years under status quo and two high-coverage screening and vaccination scenarios according to two cervical cancer simulation models
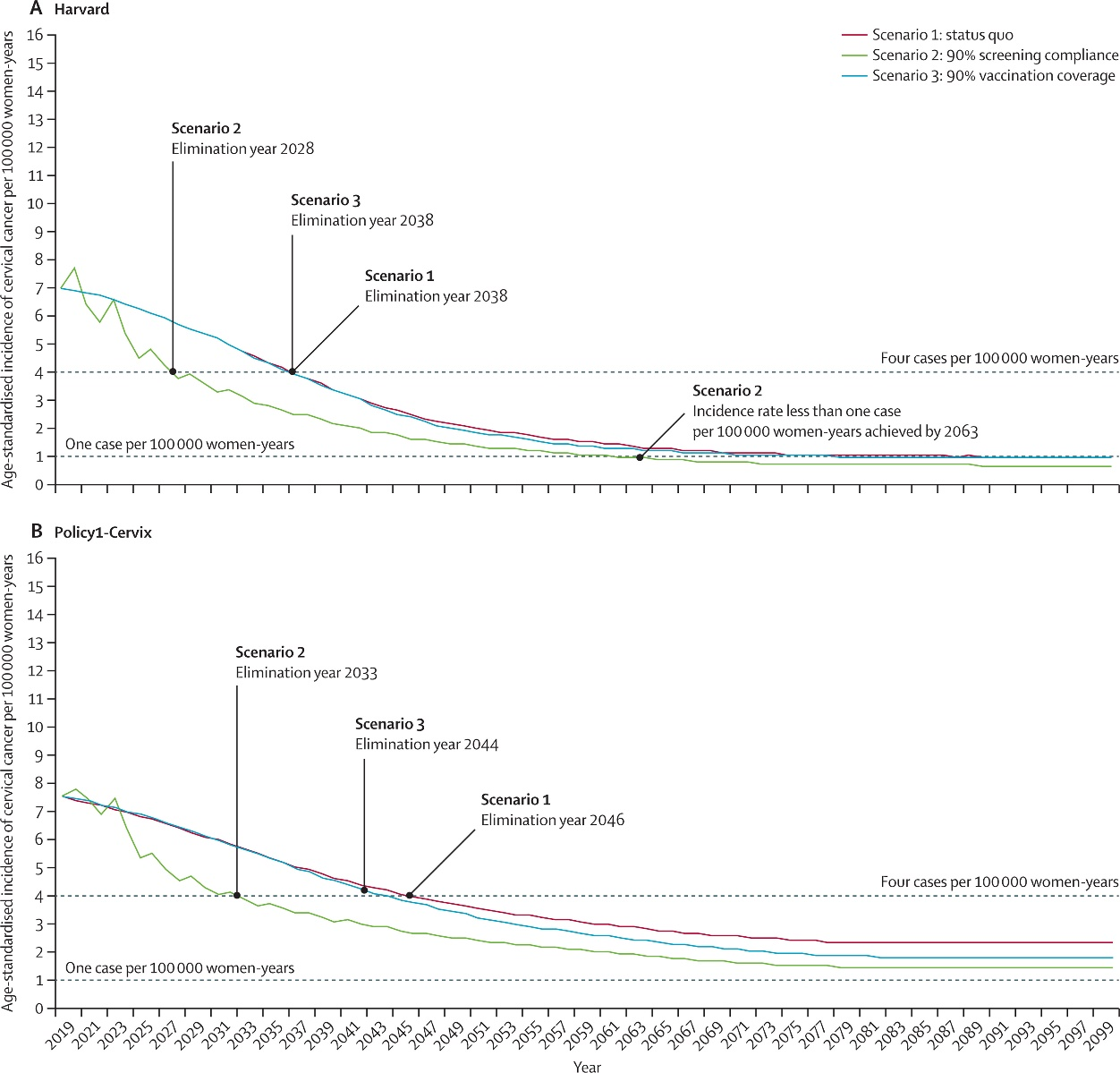
Figure 3 (Reprinted from Lancet Public Health, [vol. 5], Burger EA, Smith MA, Killen J, Sy S, Simms KT, Canfell K, Kim JJ. Projected time to elimination of cervical cancer in the USA: a comparative modelling study, e213-e222, 2020, with permission from Elsevier.)
Model Profiles & Registry
Model profiles are standardized documents that facilitate the comparison of models and their results. The Joint Profile provided includes profiles for all cervical cancer models. Individual profiles for each model are also provided and may be more current than the joint profile document.
The following model profiles have been developed by CISNET members for cervical cancer:
Model Comparison Grid (PDF, 115 KB)
Joint Profiles - all profiles combined (PDF, 8.6 MB)
Individual Models
- MGH-Cervical (MGH) (PDF, 2.8 MB)
- HSPH-Cervical (Harvard) (PDF, 4.6 MB)
- UMN-Cervical (Minnesota) (PDF, 695 KB)
- STDSIM-MISCAN-cervix (Erasmus) (PDF, 1015 KB)
- Policy1-Cervix (UYSD) (PDF, 693 KB)
Historical Versions
Individual Models
- MGH-Cervical (MGH) (PDF, 600 KB)
- HSPH-Cervical (Harvard) (PDF, 298 KB)
- UMN-Cervical (Minnesota) (PDF, 379 KB)
- STDSIM-MISCAN-cervix (Erasmus) (PDF, 739 KB)
- Policy1-Cervix (UYSD) (PDF, 236 KB)
For additional high-level information about the cervical models visit the cervical overview page on the CISNET Model Registry.