Esophageal Cancer (Historical)
The CISNET Esophageal Working Group (EWG) was funded through CISNET from 2010-2020. The EWG consisted of three distinct modeling teams focused on collaboratively modeling the incidence and mortality of esophageal adenocarcinoma (EAC) in the US population. The EWG's work has provided a strong foundation and unique opportunity to assess and improve screening and prevention strategies. The EWG has evaluated the potential of new screening technologies, prevention methods, genomic and other biomarkers, and clinical prediction tools. Precision risk stratification was used to identify an effective cancer control strategy that limits overtesting and overtreatment, thereby reducing patient burden and improving healthcare efficiency.
EWG modeling efforts have helped provide the personalized patient data necessary to construct clinical management decision aids. In addition, the EWG broadened its impact by including an esophageal squamous cell carcinoma (ESCC) natural history model and assessing ESCC screening in the US and China. The results from these research efforts have helped improve our understanding of esophageal cancer and cancer control interventions to diminish the burden of this disease in the US and globally.
Highlights
Heberle CR, Omidvari AH, Ali A, Kroep S, Kong CY, Inadomi JM, Rubenstein JH, Tramontano AC, Dowling EC, Hazelton WD, Luebeck EG, Lansdorp-Vogelaar I, Hur C. Cost Effectiveness of Screening Patients With Gastroesophageal Reflux Disease for Barrett's Esophagus With a Minimally Invasive Cell Sampling Device.Clin Gastroenterol Hepatol 2017 Sep;15(9):1397-1404.e7. Epub 2017 Feb 24.
Kroep S, Heberle CR, Curtius K, Kong CY, Lansdorp-Vogelaar I, Ali A, Wolf WA, Shaheen NJ, Spechler SJ, Rubenstein JH, Nishioka NS, Meltzer SJ, Hazelton WD, van Ballegooijen M, Tramontano AC, Gazelle GS, Luebeck EG, Inadomi JM, Hur C. Radiofrequency Ablation of Barrett's Esophagus Reduces Esophageal Adenocarcinoma Incidence and Mortality in a Comparative Modeling Analysis. Clin Gastroenterol Hepatol2017 Sep;15(9):1471-1474. Epub 2017 Jan 12.
Investigators
Controlling Esophageal Cancer: A Collaborative Modeling Project
Grant Number: U01CA199336
Abstract & Aims
Abstract: The ultimate goal of the research project is to advance our understanding of esophageal cancer and the impact of cancer control interventions to diminish the burden of this disease. This will be accomplished through a collaborative and comparative modeling project. There are two main histologic types of esophageal cancer: adenocarcinoma (EAC) and Squamous Cell Carcinoma (ESCC). Although ESCC is more common globally, in the US and much of the western world, EAC is more common and of greater concern. Esophageal AdenoCarcinoma (EAC) has experienced a remarkable (more than 6-fold) increase in incidence over the past few decades, which is largely unexplained. To date, primary screening and prevention efforts have targeted patients with symptoms of gastroesophageal reflux disease (GERD) using endoscopy and biopsy to identify patients with Barrett’s esophagus (BE), with BE patients targeted for endoscopic surveillance. There is no firm evidence indicating that this screening/surveillance strategy is effective, which is underscored by persistently poor survival rates while a large proportion of cancers continue to be diagnosed at late and invasive stages. With an estimated 40-60 million Americans with GERD and 3-12 million with BE, the management of patients who are at significantly increased risk of EAC has become an important public health issue. In addition to uncertain long-term benefits, current unproven strategies may subject patients to overtesting and overdiagnosis, negatively impacting patient quality of life while expending considerable medical resources.
The research team’s prior work includes comparative modeling of the natural history of EAC by three independent models providing a strong foundation upon which to perform analyses that assess and improve screening and prevention strategies: specifically, the evaluation of cutting-edge enhancements such as new screening technologies, prevention, genomic and other biomarkers, and clinical prediction tools. Precision risk stratification is the aim, with the broader goal to identify a cancer control strategy that is effective while limiting overtesting and overtreatment, thereby reducing patient burden and improving healthcare efficiency. These modeling efforts will provide the personalized patient data necessary to construct a decision aid, which will minimize patient screening burden by aligning management choices with personal preferences for screening. Finally, although the initial focus of the project will be on EAC, ESCC is more common and widespread globally, particularly in parts of Asia such as China. The models will be extended to include an ESCC natural history component and assess ESCC screening in the US and China. The proposal will address the overarching goals of increasing our understanding of the natural history of esophageal cancer and determining the impact and of potential cancer control interventions with the ultimate goal of ameliorating cancer morbidity.
Major Analyses & Contributions
Comparative Analyses
Predicting Trends in Esophageal Adenocarcinoma Incidence and Mortality
While esophageal squamous cell carcinoma (SCC) incidence has been declining in the US and other parts of the western world, esophageal adenocarcinoma (EAC) incidence has experienced an alarming five-fold increase over the past four decades. There is no consensus regarding the causes of this increase in EAC incidence, although an increasing prevalence of gastroesophageal reflux disease (GERD) related to increases in abdominal obesity and wider eradication of Helicobacter pylori infection have been suggested, among others. A 2014 joint analysis (Kong et al., 2014) used three independent mathematical models to analyze the EAC incidence and mortality rates among men and women aged 20-84 years in the US during 1975-2010. We then projected the EAC incidence and mortality rates to the year 2030. Despite the differences in mathematical formalisms among the three models, our projections suggest that the EAC incidence rate will continue to increase. Thus, improving screening and surveillance protocols for EAC continues to be a critical public health concern that needs to be addressed.
EAC Health States, Phases of Cancer Care, and Potential Clinical Interventions
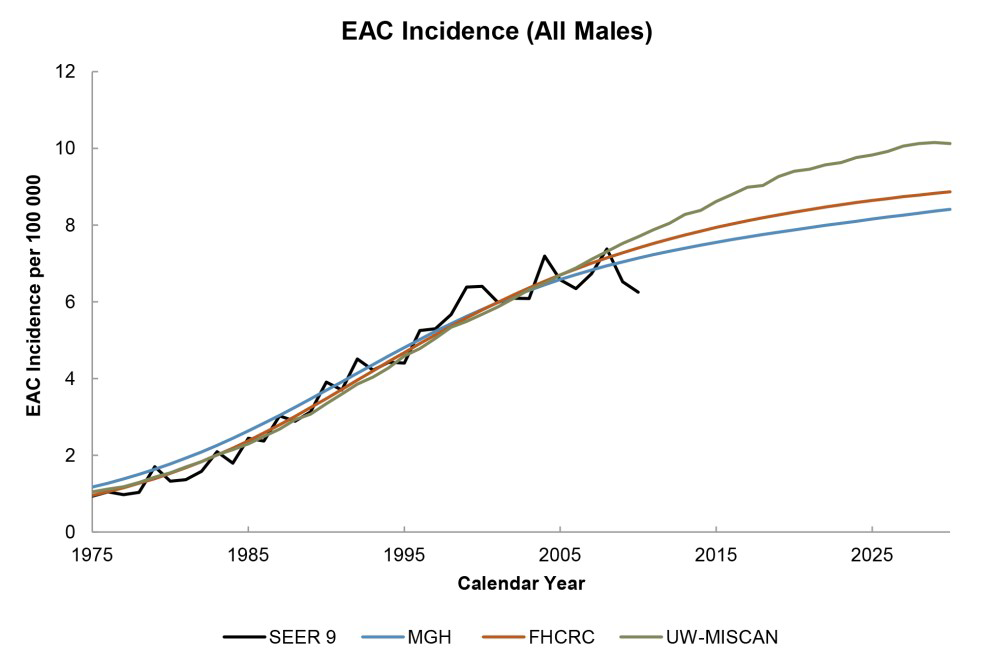
SEER EAC incidence data (black line) and projected EAC incidence rates (colored lines) for males are shown above. (Reprinted from Cancer Epidemiology Biomarkers & Prevention, 2014, Volume 23, Issue 6, pp. 997-1006, Chung Yin Kong, Sonja Kroep Curtius et al.,Exploring the Recent Trend in Esophageal Adenocarcinoma Incidence and Mortality Using Comparative Simulation Modeling, with permission from the American Association for Cancer Research.)
Evaluating the Impact of Endoscopic Ablation for Barrett’s Esophagus on Esophageal Adenocarcinoma Incidence and Mortality
Until recently, most societal guidelines recommended regular surveillance in order to achieve early
detection of EAC after diagnosis of Barrett’s Esophagus (BE). New techniques for endoscopic ablation of BE such as radiofrequency ablation (RFA) have become more widely utilized with the aim of preventing the progression to EAC. Currently the American Gastroenterological Association (AGA) guidelines recommend endoscopic ablative therapy only for patients with at least high-grade dysplasia (HGD), since the incremental benefit for this therapy on low-grade dysplasia (LGD) and particularly non-dysplastic BE patients remains uncertain and under debate. Although a growing body of investigation has focused on the efficacy and durability of RFA treatment, the impact of its widespread utilization on population-level cancer control has not been analyzed.
In this base case analysis, we applied the three CISNET models to estimate the impact of endoscopic ablative treatment on EAC mortality. We evaluated multiple management strategies, testing various factors which could impact RFA effectiveness, such as point of intervention (as determined by initial dysplasia status) and individual patient risk characteristics such as age and gender.
| Strategy | NDBE Patients | LGD Patients | HGD Patients |
|---|---|---|---|
| National History (NH) | No intervention | No intervention | No intervention |
| Surveillance (S) | 3 yearly surveillance | 6 months, Annual surveillance | 3 monthly surveillance |
| BE surveillance and HGD treatment (HGD) | 3 yearly surveillance | Yearly surveillance | Endoscopic ablative therapy |
| BE surveillance and Dysplasia treatment (LGD) | 3 yearly surveillance | Endoscopic ablative | Endoscopic ablative |
| BE treatment (BE) | Endoscopic ablative therapy | Endoscopic ablative therapy | Endoscopic ablative therapy |
| Characteristics of simulated interventions on Barretts esophagus patient cohort. BE: Barretts esophagus, ND: No dysplasia, LGD: low-grade dysplasia, HGD: high-grade dysplasia | |||
The results of our comparative simulation analyses indicated that endoscopic ablative therapy for BE can be effective for cancer control. The resources needed to achieve these results are high, especially for RFA treatment of lower grade and non-dysplastic BE where diminished efficiency limits intervention.
Analyzing current EAC targeted screening, surveillance and treatment strategy
In response to the rapid rise in EAC incidence in the US and much of the western world, the primary
cancer control measure has been to screen patients with chronic gastroesophageal reflux disease (GERD). Those identified as having BE undergo endoscopic surveillance with biopsies at regular intervals, with the goal of detecting dysplasia or early mucosally limited cancer (intramucosal carcinoma, T1a). The assumption was that this strategy would diminish EAC-associated mortality. However, the benefit of this strategy has not been demonstrated by any clinical trial. Perhaps more telling is that although this targeted screening/surveillance practice has been widely utilized for many years, there has not been an appreciable improvement in EAC incidence or survival.
We will perform a comparative modeling exercise where each of the three CISNET models will analyze the effectiveness of the current EAC control strategy, which is depicted in the figure below including management corresponding to biologic/clinical health states.
EAC Health States, Phases of Cancer Care, and Potential Clinical Interventions
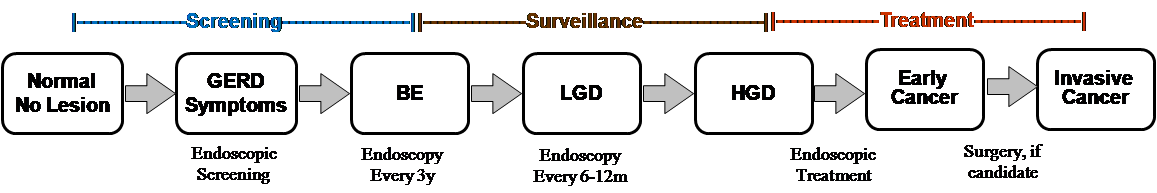
In the first phase of the modeling, we will simulate and analyze a single birth cohort. The initial birth cohort will consist of individuals born in calendar year 1930, who were 45 years old when SEER data became accurately available (1975) and were 81 years old in 2011. In the second phase, we will perform analyses from a US population perspective, as this perspective is most relevant to inform cancer control interventions and policy. All US birth cohorts from 1890-1970 will be simulated and the results aggregated to produce population results. Additionally, we will extend the analyses for the entire US population into the future (2020 and 2030) to make projections regarding the impact of these regimens on future EAC incidence and mortality. We will assess current endoscopic screening, surveillance and treatment practices to determine their projected impact in the future.
Other Achievements
Esophageal Cancer Other Achievements: Highlights
- Do trends in obesity and other lifestyle-associated risk factors match trends in Esophageal Adenocarcinoma (EAC) in three western countries?
- How do the rate-limiting steps involved in tumor initiation, malignant transformation, and progression influence the shape of the cancer incidence curve?
Do trends in obesity and other lifestyle-associated risk factors match trends in Esophageal Adenocarcinoma (EAC) in three western countries?
As obesity is a well-established factor in EAC risk, the obesity epidemic is believed to be an important driver of the rise of EAC in western countries. We aimed to test this hypothesis by comparing changes in lifestyle-associated factors with changes in EAC incidence over time between the US, Spain, and the Netherlands.
We used population-based data bases from the three countries to extract cancer incidence (US Surveillance, Epidemiology, and End Results (SEER) data base; Spain 13 cancer registries; the Netherlands Eindhoven Cancer Registry). Obesity, smoking rates, and alcohol use were gathered from national US and European health surveys or the World Health Organization (WHO) data repository).
We found that the US, Spain, and the Netherlands showed large differences in both absolute rates and time trends in EAC incidence. Time trends for obesity, smoking, and alcohol in these countries do not correlate with EAC incidence trends. Therefore, other important drivers of this increase in EAC incidence in these countries must be present. While reversing the trend in obesity is important for overall population health, reduction in EAC must rely on the identification of other causative factors. (Kroep S et al., 2014)
How do the rate-limiting steps involved in tumor initiation, malignant transformation, and progression influence the shape of the cancer incidence curve?
Cancer incidence curves harbor information about hidden processes of tumor initiation, premalignant clonal expansion, malignant transformation, and even some limited information on tumor growth before clinical detection. Our analyses of the incidences of four digestive tract cancers show that the age-specific incidence curvesupon adjustments for secular trends and, in the case of esophageal adenocarcinoma (EAC), inclusion of an event describing the conversion of normal squamous to metaplastic Barrett's epitheliumare well approximated by a model that explicitly incorporates the stochastic growth kinetics of premalignant clones, the sporadic appearance of malignant cells within these clones, and a constant time delay corresponding to the mean sojourn time of a malignant clone. While this sojourn seems very short for pancreatic cancer (3 years), intermediate for colorectal cancer (5-7 years), it is much longer for gastric cancer and esophageal adenocarcinoma (10-12 years). Furthermore, with the exception of pancreatic cancer, our results are consistent with the assumption of a high (>95%) probability of tumor stem cell extinction or terminal differentiation. We conclude that malignant clone extinction and tumor sojourn times play important roles in reducing and delaying cancer incidence and influencing the shape of incidence curves for colorectal, gastric, pancreatic, and esophageal cancers. (Luebeck EG et al., 2013)
Model Profiles & Registry
Model profiles are standardized documents that facilitate the comparison of models and their results. The Joint Profile provided includes profiles for all esophageal models. Individual profiles for each model are also provided and may be more current than the joint profile document.
The following model profiles have been developed by CISNET members for esophageal cancer:
Joint Profiles - all profiles combined (PDF, 2.0 MB)
Individual Models
- EACMo (CUIMC) (PDF, 339 KB)
- MISCAN-ESO (Erasmus/UW) (PDF, 772 KB)
- MSCE-EAC (FHCC) (PDF, 1.1 MB)
Historical Versions
Historical versions of model profiles and grids will be listed here.
For additional high-level information about the esophageal models visit the esophageal overview page on the CISNET Model Registry.